Nursing students enrolled in NUR 324 (Practicum in Medical-Surgical Nursing Practicum) and dietetic students registered in NFS444 (Nutrition and Disease) complete a interprofessional skills lab around nutrition support. Students demonstrate their knowledge in a hands-on lab through peer teaching. During the skills lab, nursing students are assigned to one of five stations. Nutrition students split up into groups and spend about 15 minutes at each station. Sandra Basley, an Assistant Clinical Professor in URI’s College of Nursing coordinates the skills lab day with Kimberly Koness, a professor in the Department of Nutrition and Food Sciences. Basley describes the skills lab as “an opportunity for nursing and nutrition students to learn about each other and from each other. Specifically, understand each others role for a patient receiving nutrition support.” Koness states,“comments from the follow up student surveys are very positive and focus as much on the collaboration with nursing students as they do on the hands on approach to providing nutrition support.”
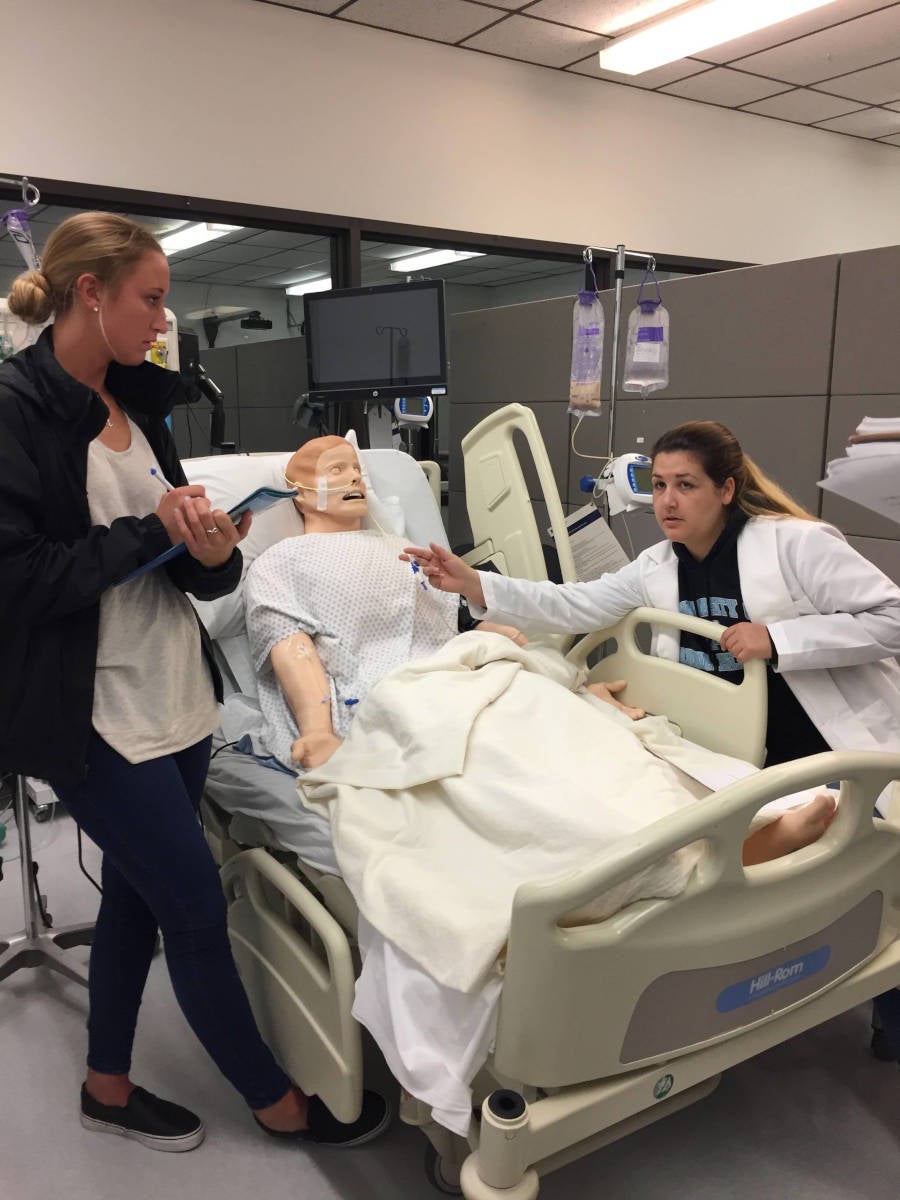
Students from both disciplines learn about the unique roles of the counter discipline as related to providing care for a patient receiving nutrition support and gain awareness of the role in each profession around administering safe and effective enteral and parenteral nutrition. Nursing students demonstrate how to properly place a nasogastric tube (NGT) feed, a tube where nutrition formula is administered through the nose and into the stomach, in an adult manikin, as well as how to assess NGT tolerance, safety, and cleanliness. By this time in the semester, nutrition students have learned about the different types of tubes, and how to assess tolerance, so seeing this in the lab helps to apply this learning. Nutrition students demonstrate to nursing students how a registered dietitian would calculate the patient’s estimated energy needs, select the appropriate tube feed formula based on the patient’s medical status, and determine the amount and rate the patient should receive the formula.
During another station nursing students show nutrition students the difference between two ways to administer nutrition directly into the veins, known as parenteral nutrition support. Nutrition students describe how a dietitian would estimate energy, carbohydrate, protein and fat needs to safely provide nutrition into the veins. Nursing students also describe the administration of tube feedings using infant and child manikins.
While only nutrition and nursing students are the two disciplines present for the skills lab, students also learn the role of the physician, nurse practitioner or physician assistant who are responsible for ordering enteral or parenteral nutrition support and approving recommendations proposed by the dietitian. Meanwhile, nurses are the ones implementing the intervention. Through the interaction between nursing and nutrition students, students are exposed to two other interprofessional practice competencies. Students learn the importance of teamwork and communication between health professions to optimize patient care. Basley also points out that holding the lab at the end of the semester allows for effective peer teaching, as at this point the skill and knowledge level for students from each respective disciplines are well-matched.
Basley plans to further expand this one-day activity. To add value to this experience, she hopes to include Nurse Practitioner and Speech Language Pathologist students, as both professions play critical roles in nutrition support. For instance, a nurse practitioner is responsible for ordering all treatment and recommendations made by the health care team, while a speech therapist is responsible for evaluating the patient’s ability to swallow and determine if it is safe for them to consume food by mouth. Basley also hopes to add an ethical element, a core IPE competency students are not exposed to during this lab. The ethical component may revolve around a case scenario of an end of life patient and if it is appropriate to continue to feed this patient via a tube feed. Such a scenario will provide the opportunity for students to come up with a solution together that is best for the patient and family. Koness is very excited about expanding this activity and involving other disciplines as well. She says taking care of patients really needs to be a team approach, and although that is taught in the classroom, it makes it more real for students when they are able to experience this in a lab setting.