‘Community First Responders program’ to educate public, provide naloxone and other resources to combat crisis
Professors, students and health professionals from the University of Rhode Island aim to stem the ongoing opioid crisis in rural communities around the state, thanks to a $1 million grant from the federal Substance Abuse and Mental Health Services Administration.
The “Community First Responders Program” seeks to educate rural communities about substance use disorder and opioid misuse, and provide resources to those communities to help address the opioid crisis, according to College of Pharmacy Clinical Associate Professor Anita Jacobson, the lead on the project, who is working with College of Nursing Professor Diane Martins and College of Environment and Life Sciences Professor Deborah Sheely.

The program involves outreach to rural communities, building upon connections URI Cooperative Extension has established through volunteer programs like the Master Gardener Program and Watershed Watch. University representatives will visit rural community events such as the Washington County Fair and 4-H meetings, teaching members of the community to recognize the signs of overdose and how to respond — including calling 911, administering naloxone and performing CPR. They will also distribute naloxone kits to combat an overdose, allowing members of the community to be true first responders.
“This is an opportunity to reach rural communities, where there is not always as much outreach regarding overdose and addiction as in more urban areas. But there is overdose risk in these communities,” Jacobson said. “We want to be a referral source and help people find the treatment and recovery they need.”
University representatives will distribute and teach residents how to use the nasal spray naloxone for victims displaying the signs of an overdose — including loss of consciousness, lack of response to stimuli, slow, shallow breathing and bluish skin, especially around the mouth and fingernails. They will also provide testing strips to check for fentanyl — one of the strongest opioids, which is sometimes illicitly added to other substances — as well as HIV/hepatitis testing, materials for referral to recovery programs, and information on methadone, buprenorphine and naltrexone treatments.
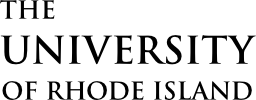
 The program also includes education to reduce the stigma associated with substance use disorder. “People are often exposed to opioids for legitimate medical reasons, and go on to develop a dependence,” Jacobson said, noting that anyone prescribed opioids should also have naloxone on hand. “Mistakes can happen. Maybe you take some Benadryl to help you sleep and that combination is too much, causing an accidental breathing emergency. You have a fire extinguisher in your house just in case a fire breaks out. Same with naloxone. Seconds really count, so you want to have it there.”
The program also includes education to reduce the stigma associated with substance use disorder. “People are often exposed to opioids for legitimate medical reasons, and go on to develop a dependence,” Jacobson said, noting that anyone prescribed opioids should also have naloxone on hand. “Mistakes can happen. Maybe you take some Benadryl to help you sleep and that combination is too much, causing an accidental breathing emergency. You have a fire extinguisher in your house just in case a fire breaks out. Same with naloxone. Seconds really count, so you want to have it there.”
Throughout the two-year project, faculty, staff members and volunteers will complete opioid misuse and substance use disorder training, and share information at dozens of public events. The Rhode to Health mobile health unit will be deployed to some events, providing resources for substance use disorder education and counseling, as well as HIV/Hepatitis C screenings.
“We want to have as many people in the community as possible to be community first responders,” Jacobson said. “If people are educated about this and know how to recognize an overdose and how to recognize if someone is caught in the cycle of substance use disorder, we can save lives.”