< Previous Article | Next Article >
Pharmacy students improve patient awareness of HPV, cervical cancer
Results of 2-year study at Clinica Esperanza/Hope Clinic found that the mostly Hispanic patients were less knowledgeable than the non-Hispanic patients about HPV, the causes of cervical cancer, and how to protect themselves from sexually transmitted diseases.
KINGSTON, R.I. – Nov. 26, 2013 – Jeff Chau didn’t know much about HPV when he started volunteering at a free health clinic in Providence three years ago. Now the University of Rhode Island pharmacy student is so knowledgeable about the cancer-causing virus he helped research and write a report on how to prevent it.
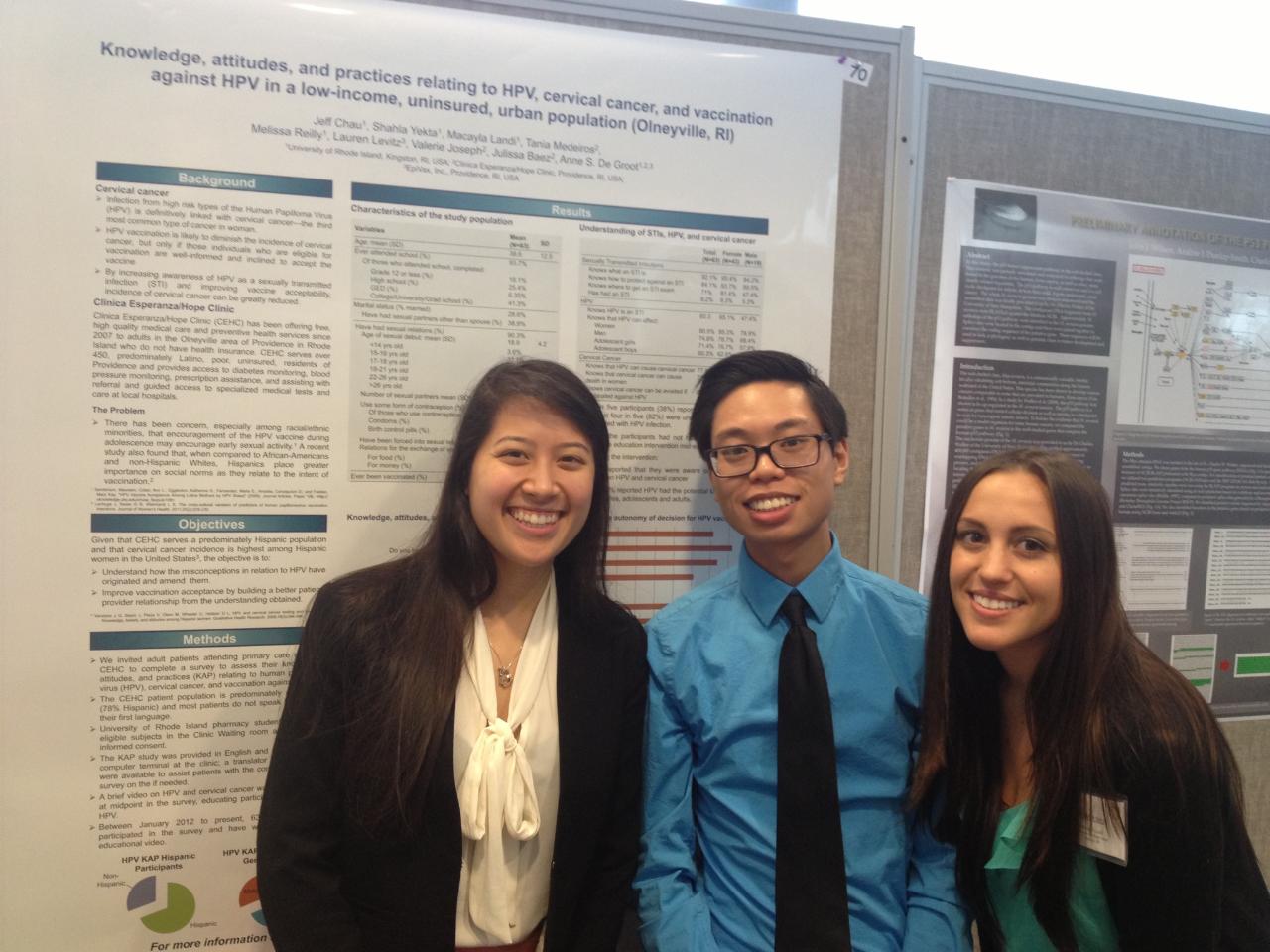
Chau ’15, of Fall River, Mass., and two other URI pharmacy students –Macayla Landi ’15, of Smithfield, and Melissa Reilly ’15, of Mahopac, N.Y. – recently completed a two-year study at the Clinica Esperanza/Hope Clinic revealing that health education plays a key role in patients’ willingness to get vaccinated against HPV. The clinic, in one of the poorest neighborhoods in Providence, provides free health care to people without insurance.
I chose pharmacy to be able to help people,’’ says Chau. “To be able to expand awareness for a particular disease and encourage people to get vaccinated was very fulfilling.
HPV, or human papillomavirus, is the most common sexually transmitted infection in the United States. Most HPV infections clear up in one to two years, but 10 percent of cases can lead to cancer of the cervix or other reproductive organs in both women and men.
The two HPV vaccines for women – Cervarix and Gardasil – have been effective at preventing the illness, resulting in a significant decrease in the number of cases. Only Gardasil has been licensed for use in males. But awareness of HPV and its link to cervical cancer and other HPV-related cancers is still lacking among low-income people with no insurance.
Chau, Landi, and Reilly surveyed 100 patients at the clinic about their knowledge of HPV and what, if anything, they do to prevent it. Shahla Yekta, a global health researcher and interim co-director of URI’s Institute for Immunology and Informatics, also helped out with the project.
At the start of the survey, patients had limited knowledge of the virus and vaccine. Halfway through the survey, patients viewed a video about the virus. After watching it, the patients said they would be more willing to get the vaccine.
Dr. Annie De Groot, founder of the clinic and research professor and director of the Institute for Immunology and Informatics, says the findings show how important it is to educate people about the illness, especially since it is preventable.


Clinica Esperanza/Hope Clinic
is a free, largely volunteer clinic in the Olneyville neighborhood in Providence’s West End.
The neighborhood has about 5,500 residents, of which 66 percent are Hispanic. The median family income for the clinic’s patients is about $19,000. The clinic offers treatment for chronic conditions such as diabetes, high blood pressure, and high cholesterol. An obstetrician / gynecologist operates a women’s clinic Friday afternoons. Is is open Tuesday and Thursday nights from 5 to 9 p.m.
To cover operating costs, the clinic depends on grants and private donations.
“After viewing the video, more than 90 percent of the patients were willing to get the HPV vaccine for themselves and their children,’’ says De Groot. “We’re encouraged by this result. The study clearly shows there’s a need to continue looking at ways to educate patients about the link between HPV and cervical cancer.’’
The study found that the mostly Hispanic patients were less knowledgeable than the non-Hispanic patients about HPV, the causes of cervical cancer, and how to protect themselves from sexually transmitted diseases.
This discrepancy, the report concluded, could be because Hispanic patients have limited access to health care and are not screened as often. They also might be reluctant to talk about sexual topics. According to the Center for Disease Control and Prevention, HPV vaccine is recommended for girls, ages 13 through 26, and for boys, ages 13 through 21.
Chau, Landi, and Reilly presented their report at the American Public Health Association meeting this month in Boston. The findings also might run in a national medical journal.
Chau says volunteering at the clinic was a life-changing experience. Initially, he signed on for one year, but decided to stay two more. He volunteered 10 hours a week, while taking on a full course load at URI.
One of the highlights was tracking down free medication for a patient who had lost her health insurance. She was a diabetic and had high cholesterol, so her drugs were crucial to keep her healthy.
“I’ll never forget the experience,’’ Chau says. “It was great sitting in on her doctor’s visit and then being able to track down free medication for her. I felt like I was doing something really worthwhile.’’
Landi also says the experience was fulfilling. “It was our first real patient interaction,’’ says Landi, a volunteer for three years. “I went into pharmacy school thinking medication, medication, and medication. But it really is about the patient. It’s great to know we really can make a difference. The HPV vaccine we’re offering can help prevent cervical cancer in our patients and that’s an amazing feeling.’’
She also enjoyed assisting patients who can’t afford health insurance. “The patients at the clinic need a health care team to help them. Without the clinic, our patients wouldn’t be able to see a doctor. The clinic really has made a difference, in both the patients’ lives and my own.’’
Reilly, a volunteer for over two years, appreciates the opportunity to give back. “It’s nice to know you’re making a difference, even in a small way.’’ One of her highlights was presenting the team’s paper to health and science groups throughout the region. “It was a great first step preparing me for my career as a pharmacist.’’
De Groot, the clinic’s volunteer medical director, says she is proud of the URI students’ work at the clinic and welcomes other student volunteers.
Photo above: Left to right: Melissa Reilly, Jeff Chau and Macayla Landi, all pharmacy students at the University of Rhode Island. The students conducted a survey and wrote a paper about the importance of educating people about getting vaccinated against HPV, a sexually transmitted virus that can cause cancer in both women and men. Photo courtesy of Dr. Annie De Groot.
Media Contact: Elizabeth Rau, 401-874-2116