Foodborne Illness Statistics
The Center for Disease Control and Prevention (CDC) estimates roughly 1 in 6 Americans (48 million people) get sick, 128,000 are hospitalized, and 3,000 die of foodborne diseases each year. Symptoms of foodborne illness include upset stomach, abdominal cramps, nausea, vomiting, diarrhea, fever, and dehydration; they can range from mild to severe and death.
Foodborne illness can affect anyone who eats contaminated food; however, certain populations are more susceptible to becoming ill with a greater severity of illness. These populations include infants and children, the elderly, pregnant women, people taking certain kinds of medications or immune suppressed (e.g., cancer patients, diabetics).
To prevent foodborne illness, it is necessary to understand how food becomes unsafe to eat and what proactive measures can be taken to keep food safe.
Causes of Foodborne Illness
The causes fall into the following 3 categories:
- Biological hazards include bacteria, viruses, and parasites. Bacteria and viruses are responsible for most foodborne illnesses. Biological hazards are the biggest threat to food safety. They can be inherent in the product or due to mishandling (e.g., time/temperature abuse).
Chemical hazards include natural toxins and chemical contaminants. Some natural toxins are associated with the food itself (i.e., certain mushrooms, PSP in molluscan shellfish), some are made by pathogens in the food when it is time/temperature abused (i.e., histamine development in certain seafood species). Some additives, such as sulfites, can be a hazard to some people. Chemical contamination can occur when products (i.e., cleaners) are not used correctly.
- Food allergens are a chemical hazard. Some people are sensitive to proteins in foods. Every food is different. Eight major food allergens include milk, eggs, fish, crustacean shellfish (lobster, crab, shrimp), wheat, soy, peanuts, tree nuts.
Physical hazards can include metal shavings from cans and plastic pieces or broken glass.
Microbiology of Foodborne Illness
Bacteria are single-celled organisms which multiply by cell division, under appropriate environmental conditions. The conditions that influence bacterial growth are the food itself, acidity, time, temperature, oxygen, and moisture. Most bacteria need nutrients to survive. They obtain these nutrients from food. Bacteria grow best in food that is neutral to slightly acidic (acidity is measured by pH). Microorganisms have different acidity (pH), temperature, and oxygen requirements for optimal growth. Bacteria need time to grow and they grow rapidly between 41°F and 140°F. Bacterial growth is slowed at temperatures below 41°F and limited at temperatures above 140°F. Some bacteria require oxygen to grow (aerobic), some grow when there is no oxygen (anaerobic), and some can grow with or without oxygen (facultative). Bacteria will grow when food and water is available. If water is bound or tied up with, for example salts or sugars, it is not available to be used by bacteria. This concept of available water is referred to as water activity (Aw).
Some bacteria can be further categorized:
- Some bacteria are spore formers. The spore protects the organism during periods of environmental stress. When the conditions become suitable, the organism germinates from the spore and continues the growth cycle.
- Some bacteria produce toxins that cause illness.
Molds are a multi-cellular fungi that reproduce by fruiting bodies that break and release thousands of microscopic mold spores, each capable of growing under the right conditions. Molds can send “roots” into the food to provide nourishment to the spore. Molds prefer damp, dark environments for optimal growth and they grow readily on almost any food, as well as walls, ceilings, and other areas of high moisture. Some molds produce toxins that can cause illness.
Viruses are the smallest known organisms. They cannot multiply in food—they need a human host. Viruses are transmitted to food from infected people.
Parasites include worms and protozoa. They cannot multiply in food; they multiply in a host cell.
Types of Foodborne Illness
Pathogens can cause different types of foodborne illness. Once a contaminated food is eaten, illness can be caused by the pathogens themselves (foodborne infection); caused by toxins produced in the food by pathogens (foodborne intoxication); and caused by toxins produced in the body by pathogens (foodborne toxin-mediated infection).
Prevention of Foodborne Illness
Follow these 4 simple steps to keep food safe:
CLEAN: Wash hands and food contact surfaces and utensils often, between tasks, and if they have become contaminated. Effective cleaning involves removing soil and debris, scrubbing with hot soapy water and rinsing, using potable/drinking water. Sanitizing involves the use of high heat (e.g., a dishwasher) or chemicals (e.g., chlorine bleach) to reduce or eliminate the number of microorganisms to a safe level.
- Wash hands with warm water and soap for 20 seconds and dry with a disposable paper towel or clean hand cloth.
- Alcohol based hand sanitizers are not a replacement for handwashing. They are not effective if the hands are dirty, they are not effective against Norovirus, and they do not eliminate all types of microorganisms.
- Wash cutting boards, dishes, and utensils after preparing each food item and before you use it for the next food.
- Use hot, soapy water, rinse with hot water, and air dry or dry with a clean paper towel or clean dish cloth.
- Or wash in the dishwasher.
- Wash countertops after preparing each food item and before you use it for the next food.
- Use paper towels or clean dish cloths to wipe kitchen surfaces or spills.
- Wash countertops with hot soapy water, rinse with hot water and air dry or dry with a clean paper towel or clean dish cloth.
- To sanitize for added protection for bacteria on surfaces, you can use the following:
- Dilute mixtures of chlorine bleach and water are a cost-effective method of sanitation. Chlorine bleach is a very effective sanitizer. It comes in several concentrations.
- If bleach is 8.25%: measure 1 teaspoon of bleach per 1 gallon of water or 1/8 teaspoon of bleach per 1 pint of water.
- Apply to the cleaned countertop and allow to sit for 1-2 minutes and air dry or dry with a clean paper towel.
- Alternatively, commercial products for sanitizing the home kitchen are available. Follow manufacturer instruction for use.
- Wash dish cloths often in a washing machine.
- Store sponge in a place so it can dry after use.
- To lower the risk of cross-contamination, sanitize the dish sponge often:
- Soak in a chlorine bleach solution for 1 min. See the following link on instructions for the bleach solution: http://msue.anr.msu.edu/news/sanitizing_kitchen_sponges
- Microwave heat a damp sponge for 1 min.
- Put sponge in dishwasher cycle.
- Replace the dish sponge often.
SEPARATE to prevent cross contamination. Cross contamination is the transfer of harmful bacteria from uncooked food products (e.g. raw meat, fish, and poultry) or unclean people, countertops, and kitchen equipment to ready-to-eat foods (e.g., fruits, vegetables, deli meats/cheeses, and prepared or cooked foods).
- Prevent cross contamination when grocery shopping.
- Physically separate raw meat, fish and poultry to prevent their juices from dripping onto other foods. This can be done by:
- Segregating raw meat, fish and poultry on one side of the shopping cart.
- Placing raw meat, fish and poultry in separate plastic bags (e.g. one bag for chicken, one bag for fish, etc.).
- Designate reusable bags for grocery shopping only. Reusable bags for raw meat, fish, or poultry should never be used for ready-to-eat products.
- Frequently wash bags. Cloth bags should be washed in a machine and machine dried or air-dried. Plastic-lined bags should be scrubbed using hot water and soap and air-dried.
- Separate raw meat, fish and poultry in disposable plastic bags before putting them in a reusable bag
- Check that both cloth and plastic-lined reusable bags are completely dry before storing.
- Prevent cross contamination when storing food in the refrigerator.
- In the refrigerator, store raw meats, fish, and poultry below ready-to-eat and cooked foods.
- When thawing frozen raw meat, fish and poultry, put the food in a plastic bag or on a plate on the lowest shelf to prevent juices from dripping onto other foods.
- After thawing in the refrigerator, food should remain safe and of good quality for a few days before cooking. Food thawed in the refrigerator can be refrozen without cooking, although quality may be impacted. See Chill section for other methods for thawing.
- Prevent cross contamination when handling, preparing, and serving food.
- Thoroughly wash your hands before and after handling different foods, after using the bathroom, and anytime they can become contaminated.
- Use separate cutting boards for meat and produce. Alternatively, prepare produce first, then meat.
- Wash and rinse cutting board, knives, and preparation area after cutting raw meat, fish or poultry. These items can be sanitized after cleaning.
- Use a clean serving plate to serve cooked meat. Do not use the plate that held the raw meat, unless it is washed.
- Throw away any sauce or dip that has been used to marinade raw meat, fish, or poultry. Do not use this extra sauce as a dip for cooked food unless it is boiled first.
COOK food thoroughly and use a thermometer to verify the proper temperature was reached.
- Cook foods to the safe minimum internal temperature, as indicated in the table below:
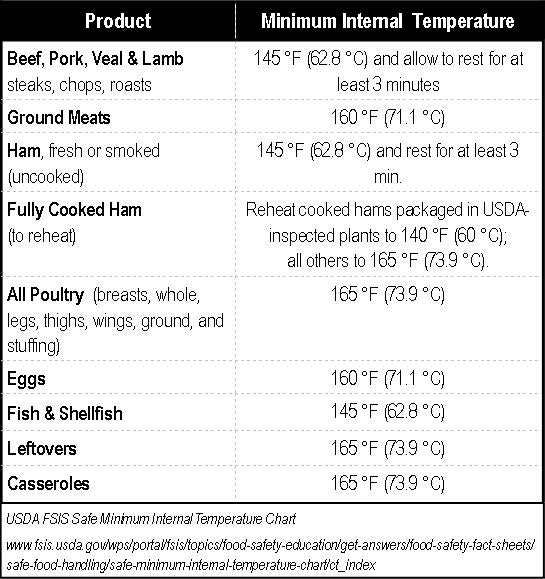
- To determine that the proper temperature was reached, place a food thermometer in the thickest part of the food and allow the it to equilibrate.
- Make sure it’s not touching bone, fat, or gristle.
- For whole poultry, insert the thermometer into the innermost part of the thigh and wing and the thickest part of the breast.
- For combination dishes, place the thermometer in the center or thickest portion.
- Egg dishes and dishes containing ground meat or poultry should be checked in several places.
- Clean your food thermometer with hot, soapy water before and after each use!
Food Thermometers – Why use them?
Not only is it important to monitor the refrigerator temperature (chill foods); but using a thermometer is the only reliable way to ensure that a food is properly cooked.
Cooking:
- Color is not a reliable indicator that the food has been cooked to the correct temperature to ensure that foodborne pathogens – bacteria, viruses – are destroyed. Determining “doneness” of hamburger cannot be safely done by looking at the brown color of the meat or of chicken by looking that the juices run clear.
- Time alone as an indicator that the food is cooked properly could result in a potential food safety hazard. Recipes may state “x minutes/pound”. However, different thicknesses of a food or ingredients that are used can alter the time needed at a specific temperature to make sure the food has reached the correct temperature to kill all pathogens.
Food thermometers come in several types and styles and range in level of technology and price. There is a lot of good information on how to use a thermometer correctly, proper placement, and how to check to see if it is accurate. Those sites are listed in the resources section.
Finally, pop-up temperature devices are commonly found in turkeys or oven roaster chickens. These devices have been around for a long time and indicate that the food has come to the correct temperature for safety. However, while these pop-up thermometers are reliable, it is often recommended that the temperature be checked in several places with a conventional thermometer to be sure.
CHILL foods promptly. Cold temperatures slow the growth of harmful bacteria. Cold air must circulate to help keep food safe, so do not over fill the refrigerator. Maintain the refrigerator temperature at 41°F or below. Place an appliance thermometer in the rear portion of the refrigerator, and monitor regularly. Maintain the freezer temperature at 0°F or below.
- Refrigerate and/or freeze meat, poultry, eggs and other perishables as soon as possible after purchasing.
- Consider using a cooler with ice or gel packs to transport perishable food.
- Perishable foods, such as cut fresh fruits or vegetables and cooked food should not sit at room temperature more than two hours before putting them in the refrigerator or freezer (one hour when the temperature is above 90°F).
- There are three safe ways to thaw food: in the refrigerator (see Separate), in cold water, and in the microwave. Food thawed in cold water or in the microwave should be cooked immediately.
- Submerging the food in cold water. It is important to place the food in a bag that will prevent the water from entering. Check the water every 30 minutes to make sure it is cold. Cook food prior to refreezing.
- Microwave thawing. Cook food immediately once thawed because some areas of the food may become warm and begin to cook during the thawing process. Cook food prior to refreezing.
- Cool leftovers quickly by dividing large amounts into shallow containers for quicker cooling in the refrigerator.
 Home
Home Browse
Browse Close
Close Events
Events Maps
Maps Email
Email Brightspace
Brightspace eCampus
eCampus